Cebranopadol
 | |
| Clinical data | |
|---|---|
| Routes of administration | Oral |
| ATC code |
|
| Pharmacokinetic data | |
| Elimination half-life | ~24 hours |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| Chemical and physical data | |
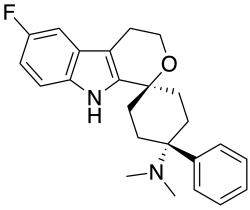
| Formula | C24H27FN2O |
| Molar mass | 378.491 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Cebranopadol (developmental code TRN-228 and formerly GRT-6005) is an investigational analgesic currently under development internationally by Tris Pharma,[1][2] a private pharmaceutical company in the United States. The drug was originally discovered and developed by Grünenthal, a German pharmaceutical company and was formerly developed by Park Therapeutics and Depomed (now Assertio Terapeutics), pharmaceutical companies in the United States, for the treatment of a variety of different acute and chronic pain states.[3][4][5] As of June 2025, phase III clinical trials have been completed for acute pain with positive results.[6]
Cebranopadol is a first-in-class dual NOP-MOP (dual NMR) agonist analgesic with a novel dual receptor mechanism that sets it apart from selective MOP agonists such as morphine. Understanding its unique pharmacology requires examining both its receptor binding profile and the functional significance of its dual agonism.
Receptor Binding Profile
Cebranopadol acts as a full agonist at two key receptors:
- μ-opioid receptor (MOP): Ki = 0.7 nM; Intrinsic Activity (IA) = 104%
- Nociceptin/orphanin FQ peptide receptor (NOP): Ki = 0.9 nM; IA = 89%
The drug also binds to other opioid receptors with lower affinity and are not believed to contribute materially to its activity:
- δ-opioid receptor: Ki = 18 nM; IA = 105%
- κ-opioid receptor: Ki = 2.6 nM; IA = 67% (partial agonist)
The Significance of Dual NOP-MOP Agonism
The dual NOP-MOP (dual NMR) mechanism is what makes Cebranopadol unique among analgesics. While opioids like morphine, oxycodone, and fentanyl act primarily through MOP receptors with no significant NOP activity (selective or preferential MOP receptoragonists), cebranopadol's balanced activation of both receptor systems creates a synergistic effect that provides for a fundamentally distinct therapeutic profile.
MOP Receptor Activity: Provides potent analgesic effects through the classical opioid pathway.
NOP Receptor Activity: Acts as a "modulator" that counteracts many of the negative side effects associated with pure MOP activation, including:
- Inhibits dopamine release, reducing the reinforcing properties that lead to abuse and addiction
- Counters the development of dependence and tolerance
- Diminishes respiratory depression risk
Pharmacokinetics
Cebranopadol demonstrates distinctive pharmacokinetic properties that differentiate it from other analgesic compounds. After oral administration of the immediate-release formulation, Cebranopadol exhibits a single dose half-life of 24 hours and a steady state half-life ranging from 62-96 hours.[7] The time to reach maximum plasma concentration occurs 4–6 hours after oral administration, with a long half-value duration of 14–15 hours.[8] The time to reach steady state is approximately 2 weeks, with an accumulation factor of approximately 2 and low peak-trough fluctuation (70–80%).[9]
Cebranopadol demonstrates distinctive pharmacokinetic properties that differentiate it from other analgesic compounds. After oral administration of the immediate-release formulation, Cebranopadol exhibits a single dose half-life of 24 hours and a steady state half-life ranging from 62-96 hours.[1] The time to reach maximum plasma concentration occurs 4–6 hours after oral administration, with a long half-value duration of 14–15 hours.[2] The time to reach steady state is approximately 2 weeks, with an accumulation factor of approximately 2 and low peak-trough fluctuation (70–80%).4 Clinical studies suggest that Cebranopadol's pharmacokinetics remain unaffected by hepatic or renal impairment, potentially eliminating the need for dose adjustments in patients with compromised liver or kidney function.[10] The extended half-life profile supports once-daily dosing regimens, which may improve patient compliance and provide more consistent pain control over extended periods compared to shorter-acting analgesics.
Analgesic Properties and Clinical Efficacy
Broad Spectrum Analgesic Activity
The dual NOP-MOP mechanism provides Cebranopadol with a broader analgesic spectrum than selective MOP agonists like oxycodone. Action at both receptor systems contributes to its antinociceptive properties across different types of pain:
Nociceptive Pain: Traditional tissue damage or inflammatory pain where MOP activation provides primary relief.
Neuropathic Pain: Nerve-related pain where the NOP component may provide enhanced efficacy compared to pure MOP agonists.
Clinical Trial Evidence
Cebranopadol has demonstrated highly potent and effective analgesia comparable to selective MOP agonists across multiple clinical settings:
Phase 2 Trials: Showed efficacy in:
- Painful diabetic peripheral neuropathy
- Chronic low back pain
- Osteoarthritis pain
- Cancer pain
Phase 3 Trials: Successfully completed acute pain studies:
- ALLEVIATE-1: post-abdominoplasty surgery pain
- ALLEVIATE-2: post-bunionectomy surgery pain
Pain Profile Advantages
Based on animal models, Cebranopadol demonstrates superior potency in neuropathic pain models compared to nociceptive pain models. This is the opposite pattern seen with selective MOP agonists, which are typically more effective for nociceptive than neuropathic pain. This suggests that the NOP component provides particular benefit for nerve-related pain conditions.
Unique Safety Profile and Abuse Potential
Cebranopadol's NOP activity leads to a very different side effect profile than seen with selective MOP agonists. Animal and dedicated human abuse potential studies suggest it has very low abuse potential and significantly less than oxycodone and tramadol.[11] Moreover, the drug has demonstrated a low risk of physical dependence and withdrawal symptoms in human trials and produces 25% less respiratory depression than oxycodone according to a press release from Tris Pharma. Additionally, Cebranopadol shows a delayed onset of respiratory effects compared to oxycodone and significantly fewer respiratory adverse events. Taken together, this data suggests the drug may have a much lower risk of addiction and overdose than selective MOP receptor agonists.
Additional Potential Benefits
Cebranopadol may differ in other respects as well. Relative to morphine, tolerance to the analgesic effects of Cebranopadol has been found to be delayed (26 days versus 11 days for complete tolerance)[3] in animal studies. In addition, unlike morphine, Cebranopadol has not been found to affect motor coordination in animals at doses in or over the dosage range for analgesia.
Research and Development History
Cebranopadol, originally developed by Grünenthal, has undergone extensive clinical evaluation with more than 33 trials encompassing over 2,300 participants. In 2015, Depomed (which later became Assertio Therapeutics) acquired licensing rights for the United States and Canada prior to Park Therapeutics acquiring worldwide rights in 2020. Park was then acquired by Tris in 2021.
Current Clinical Trial Status
As of 2025, both Phase 3 pivotal trials (ALLEVIATE-1 and ALLEVIATE-2) for acute pain have been completed with positive results:
ALLEVIATE-1 studied Cebranopadol in patients following abdominoplasty surgery
ALLEVIATE-2 studied Cebranopadol in patients following bunionectomy surgery
Both trials demonstrated statistically significant pain reduction compared to placebo with favorable safety profiles.
Regulatory Status and Future Development
The FDA granted Fast Track Designation to Cebranopadol for chronic low back pain in 2017. Tris Pharma plans to submit their NDA to the FDA in 2025 based on the completed Phase 3 acute pain studies. The company has announced plans to conduct Cebranopadol studies in multiple chronic pain indications beginning in the second half of 2025.
NIDA Grant for Opioid Use Disorder (OUD) Research
Cebranopadol has been awarded a five-year grant of up to $16.6 million from the National Institute of Drug Abuse (NIDA), a division of NIH, to study the drug for the treatment of opioid use disorder (OUD).
See also
References
- ^ Inc TP. "Tris Pharma® Announces Acquisition of Park Therapeutics - Pain Company with First-In-Class, Phase III-Ready New Chemical Entity (NCE)". www.prnewswire.com (Press release). Retrieved 2025-03-28.
- ^ "Our Pipeline". Tris Pharma. Retrieved 2025-03-28.
- ^ Linz K, Christoph T, Tzschentke TM, Koch T, Schiene K, Gautrois M, et al. (June 2014). "Cebranopadol: a novel potent analgesic nociceptin/orphanin FQ peptide and opioid receptor agonist". The Journal of Pharmacology and Experimental Therapeutics. 349 (3): 535–548. doi:10.1124/jpet.114.213694. PMID 24713140. S2CID 6942770.
- ^ Schunk S, Linz K, Hinze C, Frormann S, Oberbörsch S, Sundermann B, et al. (August 2014). "Discovery of a Potent Analgesic NOP and Opioid Receptor Agonist: Cebranopadol". ACS Medicinal Chemistry Letters. 5 (8): 857–862. doi:10.1021/ml500117c. PMC 4137374. PMID 25147603.
- ^ Lambert DG, Bird MF, Rowbotham DJ (March 2015). "Cebranopadol: a first in-class example of a nociceptin/orphanin FQ receptor and opioid receptor agonist". British Journal of Anaesthesia. 114 (3): 364–366. doi:10.1093/bja/aeu332. PMID 25248647.
- ^ rajeshlohakare@sambrown.com (2025-03-06). "Tris Pharma Announces Positive Results from ALLEVIATE-2 Phase 3 Pivotal Trial for Cebranopadol, an Investigational First-in-Class Oral Dual-NMR Agonist, for the Treatment of Moderate-to-Severe Acute Pain". Tris Pharma. Retrieved 2025-08-01.
- ^ Kleideiter E, Piana C, Wang S, Nemeth R, Gautrois M (January 2018). "Clinical Pharmacokinetic Characteristics of Cebranopadol, a Novel First-in-Class Analgesic". Clinical Pharmacokinetics. 57 (1): 31–50. doi:10.1007/s40262-017-0545-1. ISSN 1179-1926. PMC 5766727. PMID 28623508.
- ^ Ziemichod W, Kotlinska J, Gibula-Tarlowska E, Karkoszka N, Kedzierska E (2022-06-21). "Cebranopadol as a Novel Promising Agent for the Treatment of Pain". Molecules. 27 (13). Basel, Switzerland: 3987. doi:10.3390/molecules27133987. ISSN 1420-3049. PMC 9268744. PMID 35807228.
- ^ [1], KLEIDEITER, Elke; CHRISTOPH, Annette & FUSSEN, Rene et al., "Cebranopadol for treating pain in subjects with impaired hepatic and/or impaired renal function", issued 2018-07-17
- ^ [2], KLEIDEITER, Elke; CHRISTOPH, Annette & FUSSEN, Rene et al., "Cebranopadol for treating pain in subjects with impaired hepatic and/or impaired renal function", issued 2018-07-17
- ^ rajeshlohakare@sambrown.com (2022-12-13). "Tris Pharma Reports Positive Topline Data from Clinical Study of Investigational Pain Therapy Cebranopadol Showing Significantly Less Potential for Abuse Versus Tramadol and Oxycodone". Tris Pharma. Retrieved 2025-08-01.